Keywords
Abstract
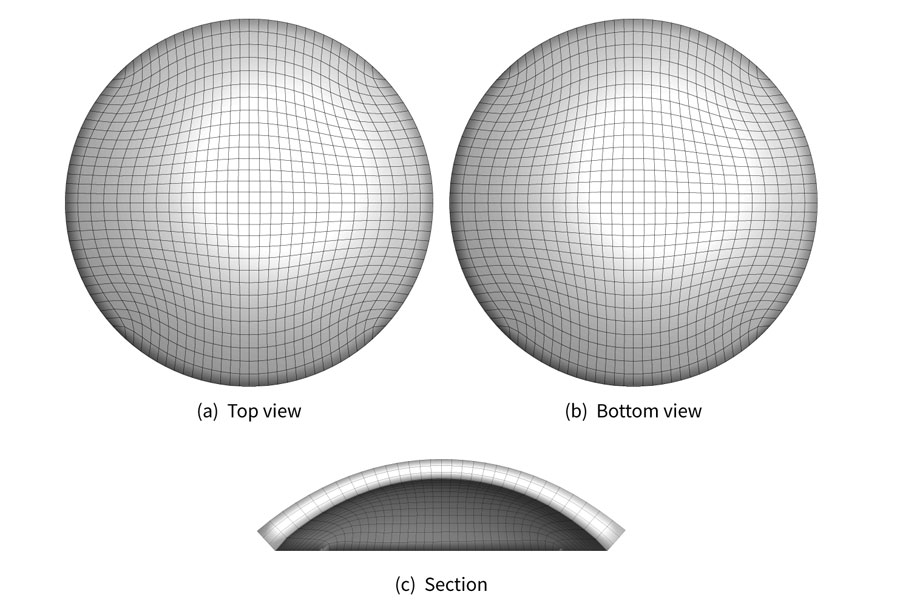
Purpose: The geometries used to conduct numerical simulations of the biomechanics of the human cornea are reconstructed from images of the physiological configuration of the system, which is not in a stress-free state because of the interaction with the surrounding tissues. If the goal of the simulation is a realistic estimation of the mechanical engagement of the system, it is mandatory to obtain a stress-free configuration to which the external actions can be applied.
Methods: Starting from a unique physiological image, the search of the stress-free configuration must be based on methods of inverse analysis. Inverse analysis assumes the knowledge of one or more geometrical configurations and, chosen a material model, obtains the optimal values of the material parameters that provide the numerical configurations closest to the physiological images. Given the multiplicity of available material models, the solution is not unique.
Results: Three exemplary material models are used in this study to demonstrate that the obtained, non-unique, stress-free configuration is indeed strongly dependent on both material model and on material parameters.
Conclusion: The likeliness of recovering the actual stress-free configuration of the human cornea can be improved by using and comparing two or more imaged configurations of the same cornea.
References
Maurice DM. The structure and transparency of the cornea. J Physiol. 1957;136(2): 263–286.
Meek KM, Blamires T, Elliot GF, Gyi TJ, Nave C. The organization of collagen fibrils in thehumancorneal stroma: a synchroton x-ray diraction study. Curr Eye Res. 1987;6, 841–846.
Daxer A, Fratzl P. Collagen fibril orientation in the human corneal stroma and its implication in keratoconus. Invest Ophthalmol Vis Sci. 1997;38, 121–129.
Munnerlyn CR, Koons SJ, Marshall J. Photorefractive keratectomy: a technique for laser refractive surgery. J Cataract Refract Surg. 1988;14(1): 46–52.
Simonini I, Pandolfi A. Customized finite element modelling of the human cornea. PLoS One. 2015;10(6):e0130426.
Boschetti F, Triacca V, Spinelli L, Pandolfi A. Mechanical Characterization of Porcine Corneas. J Biomech Eng. 2012;134(3): 031003–1–9.
Pinsky PM, Heide D van der, Chernyak D. Computational modeling of mechanical anisotropy in the cornea and sclera. J Cataract Refract Surg. 2005;31(1): 136–145.
Pandolfi A, Manganiello F. A material model for the human cornea. Biomech Model Mechanobiol. 2006;5,:237–246.
Aghamohammadzadeh H, Newton RH, Meek KM. X-ray scattering used to map the preferred collagen orientation in the human cornea and limbus. Structure. 2004;12(2): 249–256.
Quantock AJ, Boote C, Young RD, Hayes S, Tanioka H, Kawasaki S, et al. Small-angle fibre diraction studies of corneal matrix structure: a depth-profiled investigation of the human eye-bank cornea. J Appl Crystallogr. 2007;40(s1):s335–s340.
Wollensak G, Spörl E, Mazzotta C, Kalinski T, Sel S. Interlamellar cohesion aer corneal crosslinking using riboflavin and ultraviolet A light. Br J Ophthalmol. 2011;95(6): 876–880.
Petsche SJ, Chernyak D, Martiz J, Levenston ME, Pinsky PM. Depth-dependent transverse shear properties of the human corneal stroma. Invest Ophthalmol Vis Sci. 2012;53:873–880.
Meek KM, Boote C. The use of X-ray scattering techniques to quantify the orientation and distribution of collagen in the corneal stroma. Prog Retin Eye Res. 2009;28(5):369–392.
Grytz R, Downs JC. A forward incremental prestressingmethod with application to inverse parameter estimations and eye-specific simulations of posterior scleral shells. Comput Methods Appl Mech Eng. 2013;16(7):768–780.
Raghavan ML, Ma B, Fillinger MF. Non-invasive determination of zero-pressure geometry of arterial aneurysms. Ann Biomed Eng. 2006;34(9):1414–1419.
Bols J, Degroote J, Trachet B, Verhegghe B, Segers P, Vierendeels J. A computationalmethod to assess the in vivo stresses and unloaded configuration ofpatient-specific blood vessels. J Comput Appl Math. 2013;246:10–17.
Bols J, Degroote J, Trachet B, Verhegghe B, Segers P, Vierendeels J. Inverse modelling of image-based patient-specific blood vessels: zero-pressure geometry and in vivo stress incorporation. ESAIM: Math Model Num. 2013;47(4):1059–1075.
Lu J, Zhou X, Raghavan ML. Inverse elastostatic stress analysis in pre-deformed biological structures: demonstration using abdominal aortic aneurysms. J Biomech. 2007;40(3): 693–696.
De Putter S, Wolters BJ, Rutten MC, Breeuwer M, Gerritsen FA, Vosse FN Van de. Patient-specific initial wall stress in abdominal aortic aneurysms with a backward incremental method. J Biomech. 2007;40(5): 1081–1090.
Gee MW, Reeps CH, Eckstein HH, Wall WA. Prestressing in finite deformation abdominal aortic aneurysm simulation. J Biomech. 2009;42(11): 1732–1739.
Pandolfi A, Holzapfel GA. Three-dimensional modelling and computational analysis of the human cornea considering distributed collagen fiber orientation. J Biomech Eng. 2008;130:061006.
Pandolfi A, Fotia G, Manganiello F. Finite element simulations of laser refractive corneal surgery. Eng Comput. 2009;25(1):15–24.
Pandolfi A, Vasta M. Fiber distributed hyperelastic modeling of biological tissues.MechMat. 2012;44, 151–162.
Ariza-Gracia MA, Zurita JF, Piñero DP, Rodriguez-Matas JF, Calvo B. Coupled biomechanical response of the cornea assessedby non-contact tonometry.Asimulation study. PLoSOne. 2015;10(3):e0121486.
Ariza-Gracia MÁ, Zurita J, Piñero DP, Calvo B, Rodriguez-Matas JF. Automatized patient-specific methodology for numerical determination of biomechanical corneal response. Ann Biomed Eng. 2016;44(5): 1753–1772.
Ariza-Gracia MÁ, Redondo S, Llorens DP, Calvo B, Rodriguez-Matas JF. A predictive tool for determining patient-specific mechanical properties of human corneal tissue. Comput Methods Appl Mech Eng. 2017;317, 226–247.
Ariza-Gracia MÁ, Wu W, Calvo B, Malvè M, Büchler P, Rodriguez-Matas JF. Fluid-structure simulation of a general non-contact tonometry. A required complexity? Comput Methods Appl Mech Eng. 2018;
Otani T, Tanaka M. Unloaded shape identification ofhuman cornea by variational shape optimization. Comput Methods Biomech Biomed Engin. 2018;1–8.
Wollensak G, Spöerl E, Seiler T. Stress-strain measurements of human and porcine corneas after riboflavin-ultraviolet-A-induced cross-linking. J Cataract Refract Surg. 2003;29, 1780–1785.
Elsheikh A. Finite Element Modeling of Corneal Biomechanical Behavior. J Refract Surg. 2010;26(4): 289–300.
Seven I, Vahdati A, De Stefano VS, Krueger RR, Dupps WJ. Comparison of patient-specific computational modeling predictions and clinical outcomes of LASIK for myopia. Invest Ophthalmol Vis Sci. 2016;57(14):6287–6297.
Montanino A, Gizzi A, Vasta M, Angelillo M, Pandolfi A. Modeling the biomechanics of the human cornea accounting for local variations of the collagen fibril architecture. J ApplMath Mech. 2018;98(12): 2122–2134.
Studer H, Riedwyl H, Büchler P. Importance of multiple loading scenarios for the identification of material coefficients of the human cornea. Comput Methods Appl Mech Eng. 2012;15(1):93–99.
Kok S, Botha N, Inglis HM. Calibrating corneal material model parameters using only inflation data: An ill-posed problem. Int J Numer Method Biomed Eng. 2014;30(12):1460–1475.
Petsche SJ, Pinsky PM. The role of 3-D collagen organization in stromal elasticity: a model based on X-ray diffraction dataandsecondharmonic-generated images. Biomech Model Mechan. 2013;12(6): 1101–1113.
Simonini I,Pandolfi A. The influence of intraocular pressure and air jet pressure on corneal contactless tonometry tests. J Mech Behav Biomed Mater. 2016;58:75–89.
Simonini I, Angelillo M, Pandolfi A. Theoretical and numerical analysis of the corneal air puff test. J Mech Phys Solids. 2016;93:118–134.
Montanino A, Angelillo M, Pandolfi A. Modelling with a meshfree approach the cornea-aqueous humor interaction during the air puff test. J Appl Math Mech. 2018;77:205–216.
Montanino A, Angelillo M, Pandolfi A. A 3D fluid-structure interaction model of the air puff test in the human cornea. J Mech Behav Biomed Mater. 2019;94:22–31.
Sánchez P, Moutsouris K, Pandolfi A. Biomechanical and optical behavior of human corneas before and after photorefractive keratectomy. J Cataract Refract Surg. 2014;40(6):905–917.